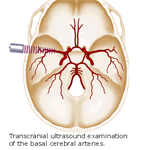
Transcranial Doppler
In performing this test, the nerve is electrically stimulated, and the electrical impulse travels through the nerve pathway and the stimulus is measured. Surface patch electrodes are used similar to those used for an electrocardiogram. They are placed on the skin over the nerve at various locations. The first electrode stimulates the nerve with a very gentle electrical impulse. The resulting electrical activity is recorded by the other electrodes. The distance between the electrodes and the time it takes for electrical impulse to travel between electrodes is used to calculate the nerve conduction velocity. If the speed is decreased , the transmission will indicate nerve disease. A nerve conduction velocity test is often performed at the same time as an electromyogram or EMG in order to exclude or detect muscle conditions.
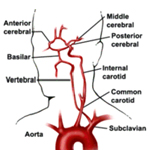
Cerebrovascular Diseases can be realistically explored and studied with the use of Transcranial Doppler. We perform a comprehensive and detailed protocol for understanding and interrogating a wide variety of neurovascular pathology:
- Carotid stenosis/occlusion
- Intracranial Stenosis
- Cerebral Emboli Detection
- Cerebral Vasospasm
- Arteriovenous Malformations
- Head Trauma
- Cerebral Circulatory Arrest
- Diminished Vasomotor Reactivity
- Reduced/Absent Cerebral Autoregulation
- Variations in Circle of Willis

TCD is relatively inexpensive, noninvasive, portable and fairly easy to use. It allows frequent repeated measurements and continuous monitoring. Immediate, real time detection of changes in cerebrovascular hemodynamics is possible. It can be utilized by any medical specialty to evaluate several neurovascular disorders.n many communities (especially rural ones), there is no neurologist and/or MRI machine available for appropriate stroke workup. In those settings and in many other places a "complete" stroke workup consists of carotid Doppler and two-dimensional echocardiogram. This misses the important evaluation of intracranial vasculature.


A TCD may be the inexpensive, simple mean to determine which patients must be referred to a specialized center for further evaluation. In addition, and in patients who decline intervention initially, TCD gives a tool for monitoring the identified lesions through the years and evaluate the effectiveness of medical treatment.
Finally, TCD may be the only mean possible to evaluate intracranial vessels in cases when other radiographic means are contraindicated. TCD is a "blind procedure"; its accuracy relies on the knowledge and experience of a trained technician and interpreter. It has limited ability to detect distal branches of intracranial vessels. In 5% to 10% of cases, sufficient penetration of the bone window cannot be achieved for ample insonation.
